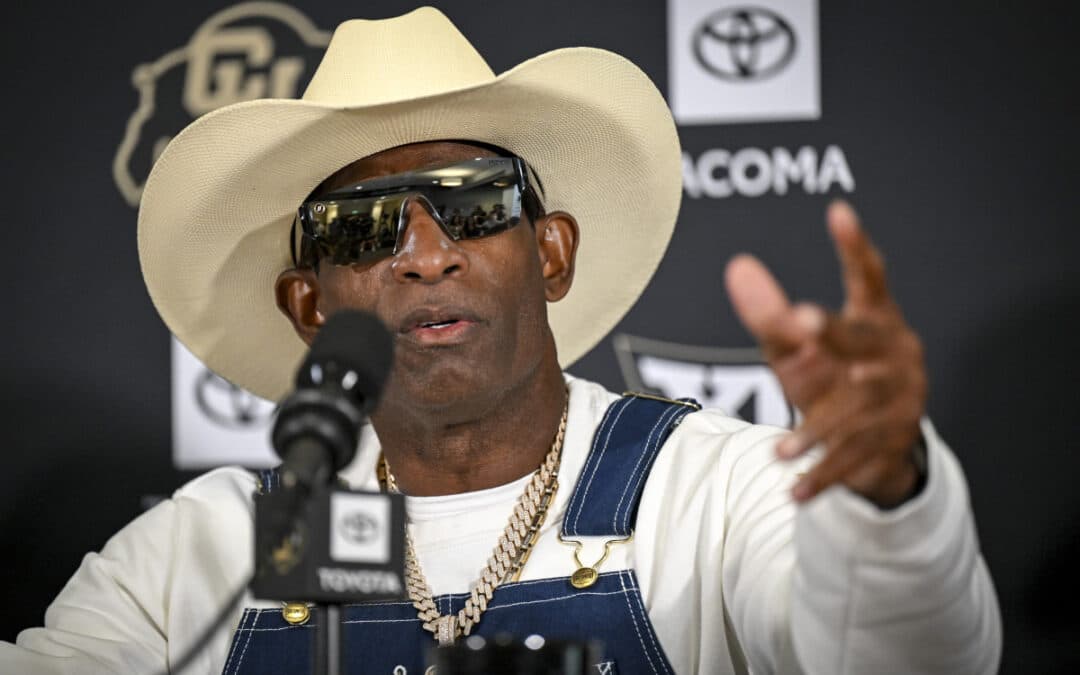
Deion Sanders’ cancer journey revealed. A revered figure in sports, Neon Deion has brought a critical conversation about cancer into the public spotlight. His candidness about his battle with bladder cancer serves as a powerful reminder for everyone to prioritize their health. Sanders’ experience underscores two vital aspects of modern cancer management: the profound impact of early detection and the transformative potential of advanced personalized strategies, such as the cryopreservation of tumor tissue and blood. These are not merely medical procedures but proactive steps that can empower individuals facing a cancer diagnosis.
The Power of Early Detection: Learning from Deion’s Story
Deion Sanders was diagnosed with an aggressive form of bladder cancer. What proved pivotal in his case was the manner of its discovery: the cancer was found during a routine annual CT scan, undertaken as a precaution due to his history of blood clots. This illustrates that early detection can occur even when symptoms are not overtly alarming or are initially attributed to other conditions. The timely identification of the tumor allowed for decisive action.
His oncologist, Dr. Janet Kukreja, highlighted the significance of this early discovery by using the word “cure,” a term she does not employ lightly in oncology, because Deion Sanders’ cancer was found before it could spread. This outcome is a compelling testament to the impact of timely diagnosis. Given the “very aggressive” nature of the tumor and its “high recurrence rate if treated within the bladder,” Sanders opted for a radical cystectomy—the surgical removal of his bladder—as a curative measure. This decision circumvented the need for years of extensive treatment that would have been necessary if the cancer had been managed less aggressively or detected at a later stage.
Sanders has since become a vocal advocate for health screenings, emphasizing, “We’re lucky to have found it at this stage where I could say the word cure”. His message, “If it can happen to Prime, baby, it can happen to you” , personalizes the call to action for regular health screenings. A public figure like Deion Sanders revealing a personal health struggle elevates public awareness far beyond what general health campaigns typically achieve. His openness about preparing a will and managing new physical changes humanizes the experience, making it relatable and impactful. When he attributes his “cure” to early detection, it creates a powerful, real-world case study for the value of routine screenings. This can lead to increased health-seeking behaviors among his vast fanbase and beyond, potentially saving lives by prompting others to get checked. This demonstrates the significant role of public advocacy in health, transforming abstract medical advice into a tangible, urgent call to action. It also subtly shifts the narrative from “cancer is a death sentence” to “early detection offers hope for cure.”
Understanding Cancer’s Comeback: The Reality of Recurrence
While early detection offers significant hope for a cure, the reality for many cancer patients is a long-term journey that often involves the risk of recurrence. As of May 2025, there are an estimated 18.6 million cancer survivors in the United States, a number projected to grow to 26.0 million by 2040. This substantial and growing population underscores that cancer management is frequently a lifelong endeavor.
The 5-year relative survival rate for all cancers combined is 69% for people diagnosed from 2014 to 2020. However, specific recurrence rates vary considerably by cancer type and stage. For instance, inflammatory breast cancer (IBC) and triple-negative breast cancer (TNBC) are more likely to recur than other breast cancer types. For breast cancer, there is a 3% to 15% chance of recurrence within 10 years with combined lumpectomy and radiation therapy, and a 25% chance if axillary lymph nodes were cancerous at initial diagnosis. The fact that Deion Sanders’ bladder cancer was described as having a “high recurrence rate if treated within the bladder” highlights this ongoing concern, even in cases of initial successful treatment.
The statistics on cancer survivorship and varying recurrence rates emphasize that for many, cancer is a chronic condition or one with a persistent risk of return. This implies that a “one-and-done” approach is often insufficient, and long-term strategies are crucial. This understanding sets the stage for the utility of cryopreservation, positioning it as a vital, proactive tool for managing the long-term, unpredictable nature of cancer, even after initial successful treatment.
The following table provides a snapshot of cancer survivorship in the U.S., illustrating the long-term journey many individuals face:
Table 1: Cancer Survivorship in the U.S. (Illustrating the Long-Term Journey)
| Metric | Data (as of 2022/2025) | Source |
| Estimated Cancer Survivors (May 2025) | 18.6 million | 5 |
| Projected Survivors by 2040 | 26.0 million | 5 |
| 5-Year Survival Rate (all cancers, 2014-2020) | 69% | 6 |
| 5+ Years Since Diagnosis (2022) | 70% of survivors | 5 |
| 10+ Years Since Diagnosis (2022) | 48% of survivors | 5 |
| 20+ Years Since Diagnosis (2022) | 19% of survivors | 5 |
| People living with metastatic bladder cancer (2025) | Expected to increase to 693,452 | 5 |
Cryopreservation: Freezing Time for Future Hope
Cryopreservation of tumor tissue and blood involves deep-freezing samples at ultra-low temperatures, typically in liquid nitrogen tanks at -196°C. At these temperatures, all biological processes cease, ensuring that the tissue and its genetic information remain viable and genetically stable for potentially decades. It is important to distinguish this process from cryoablation (also known as cryosurgery or cryotherapy), which is a treatment that uses extreme cold to destroy cancer cells directly within the body. Cryopreservation, in contrast, is about preserving biological samples for future diagnostic and therapeutic applications.
A significant advantage of preserving tumor tissue with specialized services is that patients retain ownership and control over how that tissue is used. This differs from standard pathology samples, which typically become the property of the institution. This control eliminates the immediate pressure to decide on future treatments; the tissue is stored safely, providing ample time to research options, consult with different specialists, or await new scientific breakthroughs. Furthermore, cryopreserved tumor samples contain all the delicate elements that can serve as targets for a patient’s immune system, including crucial DNA and RNA information. These elements are highly fragile and often degrade, becoming unusable for advanced analyses, if not properly cryopreserved.
The ability to store viable tissue for “potentially decades” at ultra-low temperatures, where “all biological processes cease,” effectively creates a biological time capsule of a patient’s unique cancer. This is not merely about having a sample, but about possessing a living, genetically stable representation of the disease. This stability is critical because medical science, particularly in oncology, is advancing at an exponential rate. Treatments and diagnostic tools available today may be vastly improved or entirely new in 5, 10, or 20 years. Cryopreservation thus provides a strategic advantage by allowing patients to “future-proof” their cancer care. It ensures that their most personal biological information—their tumor’s unique characteristics—remains accessible and viable for therapies and diagnostic methods that may not even exist at the time of diagnosis, offering profound hope for personalized solutions in the years to come.
Unlocking Personalized Medicine: How Cryopreservation Transforms Treatment
Cryopreservation of tumor tissue and blood is a cornerstone for the development of highly personalized cancer treatments. It offers multiple pathways to tailor therapies to an individual’s unique disease profile:
Tailored Drug Sensitivity Testing (Ex Vivo)
One of the most promising applications involves the ability to grow “organoids,” or mini-tumors, from cryopreserved tissue. These are three-dimensional cell cultures that closely mimic the structure, genetic makeup, and behavior of the original tumor, providing a highly accurate model for study. These patient-specific organoids can then be exposed to various chemotherapy drugs, targeted therapies, and experimental compounds in a laboratory setting. This
ex vivo drug screening allows researchers to observe which treatments are most effective at killing that specific patient’s cancer cells before those drugs are administered to the patient. This approach can guide oncologists toward the most promising treatments, potentially avoiding ineffective therapies and their associated side effects. It also facilitates the testing of combinations of drugs to identify synergistic effects, leading to more potent and precise treatment regimens.
Advanced Molecular Profiling
Cryopreserved tumor tissue is ideal for extracting high-quality, undegraded DNA and RNA. This is essential for comprehensive genomic (DNA), transcriptomic (RNA), and proteomic (protein) sequencing and analysis. This detailed profiling can identify specific mutations, gene fusions, protein expressions, and other biomarkers unique to the patient’s tumor. These insights are critical for guiding precision medicine drug choices, which target specific molecular pathways involved in cancer growth, and for informing prognosis. Furthermore, if future biopsies are taken, the initial cryopreserved tumor can be compared to later samples to understand how the cancer is changing over time or developing resistance to treatments, allowing for adaptive therapeutic strategies.
Paving the Way for Personalized Vaccines and Immunotherapies
Cryopreserved tissue plays a crucial role in developing personalized anti-cancer vaccines that train the patient’s immune system to recognize and attack their unique tumor cells. These vaccines utilize tumor-specific antigens—molecular information unique to an individual’s cancer cells—to create a highly targeted immune response. Advanced immunotherapies, such as T-cell based therapies (e.g., Tumor-Infiltrating Lymphocyte (TIL) therapy or Chimeric Antigen Receptor (CAR-T) modifications), often require live tumor cells or components to educate or engineer a patient’s immune cells to effectively fight their cancer.
Importantly, if tumor tissue is not available (for example, from surgery), tumor components can sometimes be derived from blood samples. These “liquid biopsies” can yield circulating tumor cells (CTC), extracellular vesicles or exosomes, or circulating tumor DNA/RNA (ctDNA/RNA), which can serve as sources of cancer antigens. This expands the accessibility of personalized vaccine approaches, ensuring that more patients can benefit from these advanced therapies. Early-phase trials, such as one for advanced kidney cancer, have demonstrated that personalized therapeutic vaccines created by examining a patient’s tumor DNA and RNA can induce successful anti-cancer immune responses, with cancer-fighting T cells remaining elevated for years. While further trials are necessary, this research highlights significant potential.
Access to Clinical Trials
Having cryopreserved tumor tissue can also make a patient eligible for specific clinical trials that require viable tissue for correlative studies or for developing trial-specific therapies. This opens doors to cutting-edge treatments and investigational approaches that might not otherwise be available, providing access to the forefront of cancer research.
The detailed benefits of cryopreservation collectively indicate a fundamental shift in cancer care. Instead of a reactive, generalized approach, cryopreservation enables a proactive, highly individualized strategy. The ability to test drugs ex vivo and develop vaccines based on patient-specific mutations means treatments can be precisely tailored, moving beyond a “one-size-fits-all” model. This minimizes trial-and-error, reduces side effects from ineffective therapies, and maximizes the chances of treatment success. This represents a move from treating “cancer” as a single disease to treating “your cancer” as a unique biological entity. It empowers patients with a level of agency and precision previously unimaginable, transforming the patient’s role from passive recipient to active participant in their long-term treatment strategy. The goal is to leverage the unique biology of each tumor to design the most effective, least toxic therapies, both currently available and those yet to be discovered.
Taking Control: Your Proactive Steps in a Cancer Diagnosis
A cancer diagnosis, while daunting, can be met with proactive measures. Cryopreservation of tumor tissue and blood is one such measure that offers a significant strategic advantage for long-term, personalized care. It is highly advisable for individuals newly diagnosed with cancer to discuss cryopreservation options with their oncologist and medical team at the time of diagnosis or surgery. This is a critical conversation for maximizing future treatment possibilities. Being an informed participant in one’s healthcare journey, asking pertinent questions, and advocating for access to advanced options like cryopreservation can profoundly impact the trajectory of cancer management. Visit the leader in tumor and blood cryopreservation at Specicare.com to learn more about how to take control of your cancer journey.
Conclusion: A Future of Personalized Cancer Care
Deion Sanders’ experience powerfully illustrates that early detection saves lives and can lead to a “cure.” However, understanding the reality of cancer recurrence underscores the need for ongoing vigilance and advanced strategies. Cryopreservation of tumor tissue and blood represents a groundbreaking step in personalized cancer care, offering a pathway to highly tailored treatments, including future personal vaccines and immunotherapies. It provides a biological blueprint for tomorrow’s medicine. Advancements in medical science, coupled with proactive patient decisions, are transforming the landscape of cancer treatment, moving closer to a future where cancer care is as unique as each individual.
Recent Comments